US scientists say they used HIV to make a gene therapy that cured eight infants of severe combined immunodeficiency, or “bubble boy” disease.
Results of the research, developed at a Tennessee hospital, were published in the New England Journal of Medicine.
The babies, born with little to no immune protection, now have fully functional immune systems.
Untreated babies with this disorder have to live in completely sterile conditions and tend to die as infants.
The gene therapy involved collecting the babies’ bone marrow and correcting the genetic defect in their DNA soon after their birth.
The “correct” gene – used to fix the defect – was inserted into an altered version of one of HIV, the virus that causes AIDS.
Researchers said most of the babies were discharged from the hospital within one month.
Dr Ewelina Mamcarz of St Jude, an author of the study, said in a statement: “These patients are toddlers now, who are responding to vaccinations and have immune systems to make all immune cells they need for protection from infections as they explore the world and live normal lives.”
“This is a first for patients with SCID-X1,” she added, referring to the most common type of SCID.
The patients were treated at St Jude Children’s Research Hospital in Memphis and at UCSF Benioff Children’s Hospital in San Francisco.
What is this syndrome?
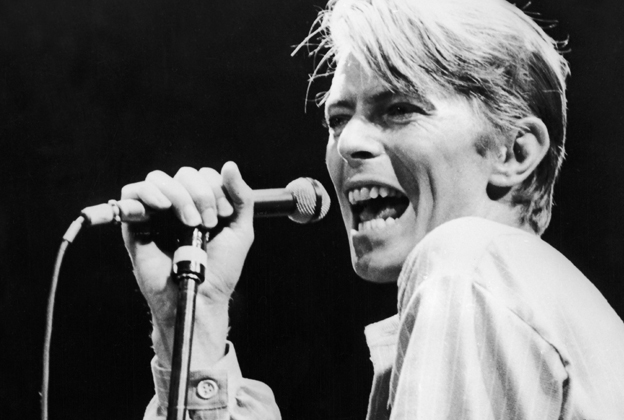
The case of David Vetter is perhaps the most famous case of severe combined immunodeficiency (SCID), a disease that made it impossible for him to engage with the world outside a plastic chamber.
Nicknamed “Bubble Boy”, Vetter was born in 1971 with the disease and died at the age of 12 after a failed bone marrow transplant.
Within 20 seconds of his birth at the Texas Children’s Hospital in Houston, he was placed in a plastic isolation chamber, where he lived until the age of six when he was given a special plastic suit designed by Nasa, the US space agency.
His parents had already lost one child to the disease before he was born.
What are other treatment options?
Currently, the best treatment for SCID-XI is a bone marrow transplant with a tissue-matched sibling donor. But according to St Jude, more than 80% of these patients lack such donors and must rely on blood stem cells from other donors.
This process is less likely to cure the bubble boy disease, and is more likely to cause serious side effects as a result of treatment.
Previous advancements in gene therapy provided alternatives to a bone marrow transplant, but these treatments sometimes involved chemotherapy and had implications for a range of other diseases, including blood disorders, sickle cell anaemia and thalassaemia, and metabolic syndrome.
Source: bbc.com